Novel Oncogene Linked to Accelerated Myeloid Leukemia Progression and Energy Production in Cancer Cells
Published on Fri Dec 29 2023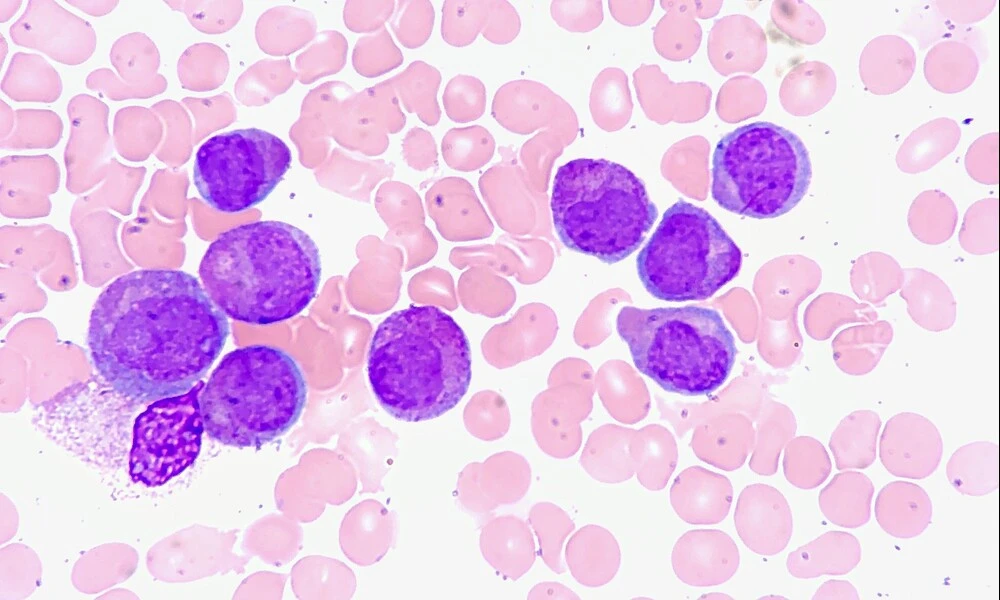 Acute Promyelocytic Leukemia, Marrow Aspirate | Ed Uthman on Flickr
Acute Promyelocytic Leukemia, Marrow Aspirate | Ed Uthman on FlickrIn a groundbreaking study, researchers have identified a novel oncogene that plays a pivotal role in the progression of myeloid leukemia. Chronic myeloid leukemia (CML) is a type of cancer that starts in the blood-forming cells of the bone marrow. While drugs such as Gleevec have revolutionized the treatment of CML, patients in the later, more aggressive "blast crisis" phase of the disease remain difficult to treat effectively. The study could open new avenues for therapy.
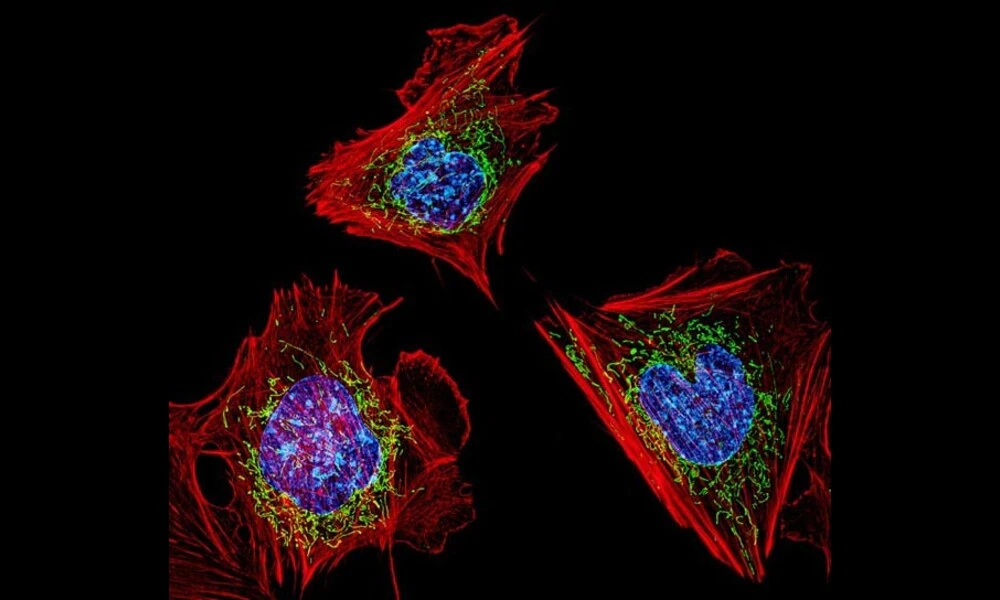
The researchers discovered that a translocation involving the Musashi2 (MSI2) protein, when combined with the most common genetic change associated with CML—the BCR-ABL fusion—can drive the disease into its more lethal form. The term "translocation" refers to an event where a piece of one chromosome breaks off and reattaches to another, which can disrupt and fuse genes, sometimes leading to cancer. In this instance, the fusion of MSI2 with another gene, HOXA9, not only accelerates disease progression but also enhances the cancer cells' energy production by affecting mitochondrial function—cellular structures that produce most of our cellular energy.
The findings, if confirmed by subsequent research, may not only provide new insight into the mechanisms involved in the transition from chronic leukemia to blast crisis, but could also reveal potential targets to combat drug resistance and improve patient outcomes. Importantly, this translocation is the first to involve MSI2 and suggests that it could play a role across other forms of cancer as well, offering a profound potential impact on how we understand and approach the treatment of various cancers.
For those battling myeloid leukemias, particularly in advanced stages, this research is an encouraging beacon, offering hope by providing a deeper understanding of disease mechanics. As this advanced phase of the disease often carries poor prognoses, this discovery is immensely valuable for clinicians and researchers. It lays the groundwork for future studies and, eventually, may lead to novel and more effective treatment strategies that specifically target these newly identified oncogenes and their downstream effects. The full paper detailing the study’s nuanced findings can be accessed through the bioRxiv preprint server via the link below.
Keep Reading
ChatGPT surpasses crowd-workers in text annotations, revolutionizing data annotations and classification. Cost-effective and highly accurate. #AI #TextAnnotation